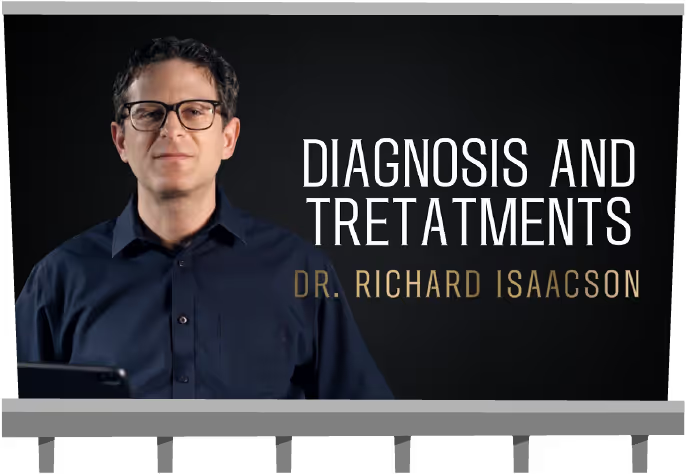





Section 4
Buckle Up: Living with Dementia
Understanding Behaviors and Tips for Managing Them
What are dementia-related behaviors?
Remember, if you’ve seen one case of dementia, you’ve seen one case of dementia. Everyone is different, but here are some behavioral bumps in the road that are common to the different stages of dementia:

%201.svg)
%202.svg)
What triggers dementia-related behaviors?
Behaviors most often stem from three different buckets of triggers: emotional, physical, and environmental. If we can identify and appropriately manage the trigger, we have a better chance of keeping those behaviors from escalating:
Emotional
Physical
Environmental
Emotional
FRUSTRATION
DISORIENTATION
LONELINESS
FEAR
BOREDOM
ANXIETY
Physical
HALLUCINATIONS
DELUSIONS
SLEEP ISSUES
PAIN
URINARY TRACT INFECTION
DEHYDRATION
Environmental
OVERSTIMULATION
CARE PARTNER’S APPROACH
UNMET PERSONAL NEEDS
MEDICATION MANAGEMENT
FEELING ISOLATED
FEELING RESTRICTED


For example:
Every day at 3pm, Mom gets ready to pick up the kids from school. Problem is: you’re her kid, and you’re 42. It's challenging to redirect her as she becomes adamant that she will be late. Knowing that 3pm is a trigger time, encourage a snack and a pleasurable activity at 2:30, that can distract and redirect from the 3pm trigger.

How to recognize dementia-related behaviors and determine if they are expressions of unmet needs:
It’s important to explore dementia-related behaviors as the possible expression of unmet needs. Likely, your person’s goal is not to drive you crazy but to express themselves, which can get increasingly challenging as the disease progresses.
Think of it this way - if you, as you are today, had a word at the tip of your tongue, you can tell someone “ooh, it’s on the tip of my tongue.” If you had a dementia, and you were trying to express yourself, and the words didn’t come out right, and you couldn’t tell someone, you might show them your frustration. In the absence of words, we act.



There’s a ton of information out there when it comes to understanding dementia-related behaviors. We know you’re busy, so we found the best of the best resources for you.

Non-pharmacological approaches to managing behaviors:
Non-pharma-what? Non-pharmacological approaches are those that do not involve the use of medication.
Examples of non-pharmacological approaches include:
Behavioral Modifications (establishing a structured daily routine)
Environmental Modifications (reducing noise or removing hazards)
Cognitive Stimulation (puzzles, memory games, reminiscence therapy)
Art, Music, and Other Creative Therapies
Pet Therapy
Sensory Stimulation (aromatherapy, massage)
Physical Exercise
Social Engagement
Caregiver Education and Training
Pharmacological approaches to managing behaviors:
You guessed it, this means approaches that include medication. If non-pharmacological interventions have been exhausted and behaviors are severe enough to impact your person’s quality of life or safety, medication could come into play. It's very important that at this stage, should you enter it, your person’s medications are carefully and continuously monitored and adjusted with the help of a healthcare professional. The potential benefits of medication should always be weighed against the potential risks and side effects.
Some common pharmacological approaches to dementia-related behaviors include:
Antipsychotic Medications (to manage agitation, aggression, and psychosis)
Antidepressant Medications (to manage depression, anxiety, and agitation)
Sedative-Hypnotics (to manage sleep disturbances)
There are other drugs that are primarily used to treat the cognitive (vs. behavioral) symptoms of ADRD. While they do not specifically target behaviors, improving cognitive function may indirectly reduce some behavioral symptoms.

Changing Care Needs
We’ve said it before, but it’s worth repeating, dementia is not a one-size-fits-all condition. It’s different for everyone and even for each individual, the road changes constantly. One step toward not totally freaking out is learning to manage expectations: there WILL be MANY changes as time goes on.
Quick Tips for Managing Change:
Having ongoing, open conversations with the medical professionals on your squad.
Find a way to track your person’s changes over time that’s easy for you. It might be a journal that you and other members of your squad use to write daily entries so you can spot trends. Or, you can use an online platform such as CareVirtue to enter daily journals and updates, tag the behaviors, and rate days using an emoji scale. You can even run a search based on all of the smiley faces or frownie faces and export those entries for your healthcare team.
Be honest with yourself about what your person needs, what you are willing to do, and what you are capable of doing.
Give yourself permission to ask for help.



Restroom Support & Assistance
In health care, “toileting” is the act of assisting someone with their elimination needs. But let’s be real, who uses “toileting” at home? So here, we’ll refer to this part of caregiving as “restroom support.” Restroom support, assistance, and hygiene are really personal. Struggling with these can make your loved one feel like they’re losing control, which can be tough on their self-esteem and dignity. Since restroom assistance is such a big part of feeling independent, and such an intimate thing, it can be hard for them to accept help, especially from someone they’re close to. That’s why it’s important to approach restroom support with understanding and keep the communication open.
Common restroom concerns among people living with dementia
Urinary tract infections (UTIs)
UTIs happen when bacteria get into the urinary tract, and they’re a pretty common but serious health issue, especially for folks with dementia. The tricky part is that dementia can make it hard for them to recognize or communicate UTI symptoms, which often leads to delays in getting help. If a UTI goes untreated, it can cause sudden confusion and changes in behavior, like more agitation or withdrawal, and it can even speed up the progression of dementia. That’s why it’s super important to spot UTI symptoms early and get medical help right away.
Pain, burning sensation during urination
Urgency to pass urine
Feeling of not being able to fully urinate
Cloudy, bloody, or bad-smelling urine
Lower abdominal pain
Urinary incontinence
Mild to high fever
Delirium/acute confusion
Nausea or vomiting
Shaking or chills
Loin pain
Flank tenderness

Incontinence is when someone can’t control the leakage of urine, feces, or both. Urinary incontinence can be anything from small leaks and dribbles after using the bathroom to a complete loss of bladder control. Fecal incontinence can range from passing a little bit of feces when passing gas to a total loss of bowel control. This can really affect physical health, dignity, and overall quality of life.
With dementia, it can get even more complicated. It can make it hard to recognize the need to go, remember where the bathroom is, or communicate that they need help. Sometimes, when communication is tough, they might not be able to tell you they need to use the bathroom. Dementia can also make it tricky to recognize, find, or use the toilet properly.
%201.svg)





Proactive Steps
The embarrassment after an accident might make your person hesitant to ask for help, and they might even start avoiding the bathroom altogether. If an accident happens, it’s important to remember that it’s not their fault. Try to help them move past any embarrassment or distress, and do your best not to show anger or frustration. It can be tough, so if you’re finding it hard to manage your feelings about incontinence, don’t hesitate to reach out to a health professional for some support.
Promoting Bladder and Bowel Health
Taking care of bladder and bowel health in someone with dementia means looking after both the body and mind. Here are some tips that can help:
Adequate Hydration: Make sure they’re drinking 6-8 glasses of fluids each day. Staying hydrated helps prevent constipation and UTIs. Water is the best option, but other fluids work too if needed (for example, Jello, popsicles, soups, coconut water, fruits, fruit infused water, smoothies, etc.)
Balanced Diet: Offer a diet full of fiber, like fruits, veggies, and whole grains. Fiber is great for keeping bowel movements regular and preventing constipation.
Regular Exercise or Movement: Encourage them to stay active with things like walking or gentle exercises. It’s good for overall health and supports bowel function. Pelvic floor exercises can also help with bladder control. There are also pelvic health specialists andOccupational Therapists who can assist.
Accessible Bathrooms: Make sure the bathroom is easy to find and use. Keep it well-lit, clearly marked, and free of obstacles. Adding grab bars, raised toilet seats, and other aids can make it safer.
Easy-to-Remove Clothing: Go for clothing with elastic waistbands, Velcro, or other easy-to-remove fastenings to make bathroom trips quicker and easier.
Routine and Assistance
Setting up a toileting routine can really help someone with dementia. It might be useful to create a timetable for reminders about when to use the bathroom. You could list times like when they wake up, before each meal, at coffee/tea times, and before bed. You can also set up reminders to prompt them to use the bathroom or check if their pad needs changing. When you’re helping out, it’s good to remind them every 2-3 hours to use the toilet. Be sure to communicate this schedule with your entire care team as well, so everyone is on the same page.
Supporting Bathroom Needs at Night
A person with dementia might wake up feeling disoriented and struggle to find the bathroom quickly. Here are a few ideas to make things easier:
.svg)
Dealing with restroom issues and incontinence can make going out more challenging, but staying social is important. Feeling confident and prepared can help prevent giving up on activities or feeling isolated. To make traveling or being out and about easier, plan ahead—like finding accessible toilets in advance. Be ready by carrying a light pad (the kind that attaches to underwear), spare clothing, extra pads, and a bag for soiled items.
Give regular reminders about using the toilet. Use Alexa or smart devices if accessible to set reminders. Place a note next to the timer or buzzer explaining what to do when it goes off.
Hand them toilet paper when needed. They might need a bit of help getting it started. Wipes can sometimes be easier to use than toilet paper.
Don’t rush them—take it slow.
Give them as much privacy and modesty as you can.
Try double voiding, which means having them pass urine more than once each time they go to make sure their bladder is completely empty.
Help them find the toilet with a sign on the door that has both words and a picture. Make sure it’s bright and easy to see. Leave the toilet lid open when it’s not in use.
Plug in night lights so they can see a clear pathway to the bathroom.
Watch out for mirrors in the bathroom; they might confuse their reflection for someone else.
Keep the path clear of obstacles and move any furniture that’s in the way. Open any doors they might find hard to open.
Take a look at the bathroom atmosphere: Is it too busy and cluttered, potentially causing a trip hazard? Is it too beige or muted, making it hard to identify the toilet?
Consider working with a home safety specialist or Occupational Therapist for guidance.


It’s important to keep an eye out for signs that your loved one might need to use the restroom, especially if they’re having trouble communicating clearly. Look for things like:
Agitation
Fidgeting
Pacing
Facial Grimacing
Getting up and down a lot
Pulling at their clothes
Wandering around
Touching their genital area




Consult Healthcare Professionals
Team up with doctors, nurses, and occupational therapists to come up with personalized strategies for managing bladder and bowel health. They can give you specific advice and support based on what your loved one needs.
Continence aids can be used to help keep your loved one comfortable as well as protect clothing, furniture, and bedding.
Hygiene and Skin Care
Proper Hygiene: Help teach and assist with good hygiene practices to prevent UTIs and skin infections. Use gentle, unscented products to avoid irritation.
Protective Products: Use absorbent pads, adult diapers, or other protective items to manage incontinence and keep things clean.
Monitoring and Medical Care
Monitor for UTIs: Keep an eye out for signs of UTIs, like sudden changes in behavior, increased confusion, agitation, or discomfort when urinating. If you suspect a UTI, get medical help right away.
Regular Health Checks: Schedule regular visits with healthcare providers to keep track of bladder and bowel health, review medications, and address any new issues.
Communication and Support
Clear Communication: Use simple, clear instructions and offer gentle reminders about using the toilet. Stay calm and supportive.
Understanding and Patience: Be patient and empathetic, knowing that incontinence can be a tough and sensitive issue. Provide reassurance and try not to show frustration or anger.
Flexibility: Be flexible and know that your person might refuse bathroom assistance. This doesn’t mean they do not have a need to actually go. Take a breather, and try to reapproach the situation several minutes later, with a different method.
The most common type of urinary incontinence for people with dementia is an overactive bladder, which means they might have a sudden, intense urge to urinate and need to go frequently.
Preventing incontinence means taking a proactive approach with regular bathroom schedules, staying hydrated, eating a balanced diet, and keeping up with good hygiene. Managing incontinence well can help reduce the risk of skin infections and UTIs, making things more comfortable and preserving their dignity.



Changing Care Settings:
As your person’s needs change, their setting may need to change accordingly. Here are some common care settings:
Day Programs
Day programs can be great for social engagement, and a break for you. Many include meals and organized activities tailored to the needs of people with ADRD. Read more:
A Guide to Memory Care Day Centers
Memory Cafes
Is this really a thing? YES! And if you can find one along your journey, it might be worth the stop! Memory Cafes are designed specifically for individuals with Alzheimer’s Disease or any other form of dementia, or other brain disorders. Cafes are also set up to provide a space and a break for care partners too. Learn more and see if there is one near you!
Residential Settings
Residential settings include nursing homes, assisted living, memory care, and group homes. Residential settings provide a high level of care and can reduce the burden on care partners. While this isn’t always an easy or affordable option, it can improve the quality of life for everyone involved.
Assisted Living Locators
These services specialize in helping you navigate the often complex and overwhelming process of finding appropriate living arrangements. In short: they do the leg work for you. They will research your options, make appointments for tours, and help get answers to your questions. In most places, Assisted Living Locators are independently run companies, so you might pay an initial screening fee. Then, if you choose one of the places your locator found for you, they receive a finding fee from the facility - so they are incentivized to make a good match for you. As always, do your homework before contracting with someone. The Better Business Bureau is always a good resource to check a company’s credentials. You can also ask for references!
Get Started:
Assisted Living Locator


%201%201.svg)


Nutrition & Hydration

What is your guiltiest pleasure, only-on-a-road-trip snack of choice?
(Okay, this isn’t a quiz, we just want to know.)


Poor nutrition for individuals with dementia is like a road trip without snacks. Unthinkable!


Tips for maintaining the health and well-being of your person via nutrition.
Maintain a Routine:
Establish regular meal and snack times to provide structure and predictability, which can help reduce anxiety and confusion.
Balanced Diet:
Aim for a balanced diet that includes a variety of foods from different food groups, including fruits, vegetables, lean proteins, whole grains, and dairy products.
Texture-Modified Foods:
As dementia progresses, individuals may have difficulty with chewing and swallowing. Consult a speech therapist or dietitian for guidance on texture-modified diets, such as pureed or soft foods, to prevent choking or aspiration.
Hydration:
Encourage regular fluid intake to prevent dehydration. Some individuals with dementia may forget to drink, so offer fluids throughout the day, including water, juice, and soups.
Finger Foods:
Offer easy-to-eat finger foods like cut-up fruits, vegetables, or sandwiches to make eating more manageable for those with motor skill difficulties.
Minimize Distractions:
Create a calm and quiet dining environment to reduce distractions, which can help individuals focus on their meals.
Adapt to Preferences:
Cater to the person's preferences and cultural background when planning meals. Familiar and favorite foods can be comforting and encourage eating.
Supplements:
Some individuals may benefit from vitamin or mineral supplements, but these should be recommended by a healthcare provider.
Monitor Weight:
Keep an eye on your person’s weight. Weight loss is common in dementia, but shouldn’t be ignored. Consult a healthcare professional if significant weight loss - or gain - occurs.
Food Safety:
Ensure that the food is safe to eat by checking expiration dates and maintaining proper food storage and hygiene practices.
Special Diets:
If the individual has specific dietary restrictions or medical conditions, work with a healthcare provider or dietitian to develop a suitable meal plan.
Medication Interactions:
Be aware of any medication interactions with food. Some medications may require adjustments in meal timing or type of food consumed.
Be Patient:
Eating can become a slower and more challenging process for individuals with dementia. Be patient, and avoid rushing or pressuring them to eat quickly.
Regular Dental Care:
Good oral hygiene and regular dental check-ups are essential for maintaining oral health, which can impact eating abilities.
Did you know that
oral health = heart health = brain health?
Research suggests there is a link between poor oral health and cardiovascular disease. Bacteria in the mouth can travel through the bloodstream and potentially contribute to the development of conditions like endocarditis (infection of the heart's inner lining) and atherosclerosis (clogged arteries). The inflammation and infections associated with gum disease, in particular, can exacerbate heart health issues.
Emerging research is also exploring connections between oral health and brain health. Some studies suggest that chronic gum disease and inflammation may be associated with a higher risk of cognitive decline and conditions like ADRD. The exact mechanisms of this relationship are still TBD, but it’s safe to say that a healthy mouth could support a healthy brain. So, schedule that cleaning!

Record and Observe:
Keep a food diary to track eating habits and identify any patterns or changes in appetite. Share this information with healthcare providers.
Seek Professional Help:
If you have concerns about the individual's nutrition, seek guidance from a registered dietitian or healthcare professional who specializes in dementia care.


Managing Mealtime
When it comes to mealtime with your person, it’s not just about what’s on the plate. Setting up a routine and creating good vibes around mealtime can make all the difference. Here are three key things to keep in mind:
Pick a time when they’re feeling calm and alert. That’s when you’ll have the most success.
Share the meal together. It’s a perfect chance to connect, and when they see you eating, it might nudge them to do the same.
Keep it simple and soothing.
Turn off the TV and radio to cut down on noise, or maybe play some soft music in the background.
Clear the table of any clutter like extra utensils or condiments, and steer clear of busy patterns.
Stay patient and relaxed, even if it takes a bit longer.
Make sure the room is well-lit.




A Note on Tableware & Utensils
Here’s a handy tip: using tableware that contrasts with the food can actually help your person eat more. Think red plates and bowls—they make the food pop and easier to see. Skip the patterned plates, though; they can be confusing.
When it comes to utensils, go for ones that are easy to hold. And as time goes on, you might find that bowls work better than plates, and spoons are easier to manage than forks. There are specialty utensils that can be used. Speak with a medical provider and OT for suggestions. Don’t hesitate to let them eat with their fingers if that’s easier—getting enough nutrition is what really matters.
And one more thing: steer clear of sharp knives to keep things safe.
Unique Ways to Encourage Water Intake
Keeping hydrated is super important, so try offering small glasses of water throughout the day. Brightly colored cups that are easy to hold are a great choice—whether or not they have lids depends on what your person needs. Bendable straws can be a big help too.
You can also sneak in some extra hydration with foods that have high water content, like fruits, soups, milkshakes, and smoothies.
Here are some products designed to make mealtime easier.
Dysphagia (difficulty swallowing)
At some point, almost everyone with dementia will have trouble swallowing. This can make meals and staying hydrated really tough and stressful. If you notice your loved one struggling with swallowing, it’s important to reach out to their healthcare provider. Speech therapists and occupational therapists can also help you make adjustments to mealtime.
What to look for
Drooling saliva, food or fluid
Effortful or prolonged chewing
Pocketing of food in cheeks
Pooling of fluid in mouth
Spitting out food
Nasal regurgitation
Fatigue
Coughing when drinking or eating
Wet or gurgly voice
Food getting stuck in the throat or neck region
Pain or discomfort with swallowing
Unexplained weight loss
Chest infections or aspiration pneumonia - when food or liquid goes into the lungs





Ways to manage dysphagia
You might need to change the texture of food and drinks—think soft, minced, pureed, or thickened. A speech pathologist can help figure out the right consistency for your loved one.
Sit beside and slightly in front of your loved one, so you’re at eye level.
Positioning is key: their head should face forward and be slightly tilted forward (if it tilts back, it can open the airway and increase the risk of choking). Make sure their body is upright and centered, not leaning to one side. Their pelvis, buttocks, and back should touch the back of the chair to prevent slipping forward. Hips, knees, and ankles should be at a 90-degree angle.
Try placing food in the middle of their tongue to help them manage it better. Feed slowly, giving them enough time to swallow.
Try hand under hand techniques (Teepa Snow), to ensure you are not force-feeding. This can help your person maintain dignity, while also ensuring that meal time is still an activity they can enjoy using their maintained skills & independence. Think “do with, not do for!” Be aware that utensils can be perceived as random objects so a hand-under-hand approach keeps your person involved in mealtime.
Keep an eye on their Adam’s apple to ensure they’re swallowing properly.

What to do when your person says they aren’t hungry/already ate
Meet them where they are. Say, “Oh I’m sorry!! I did not know you already ate.” And re-approach the situation in another 10-15min. Try not to keep pushing them to eat in that moment which could upset them more.
When serving meals, keep servings smaller so as not to crowd the plate. Too much food can look overwhelming and discourage eating.
Can your person visually see the food? Make adjustments to ensure eating is accessible and no barriers to getting the food from plate to mouth.
OR they say they are still hungry
Try not to say “You already ate! Remember?” Because, well, maybe they don’t and this doesn’t actually solve the problem.
Appetite and taste acuity change as we age. Your person may actually still be hungry. Consider offering healthy snack items in small portions.
Finger foods that are easy to grab and go can encourage healthy snacking & keep your person satisfied.
Give yourself grace and try not to take it personally. Your person may accuse you of not feeding them, but it’s not them talking- it’s the dementia. Get support to help you manage the emotions.

Hey what about ME?
Whether you share genes with the person you’re caring for or not, you may be wondering, “how do I protect MY brain?” Well, good news. You can do both at once! Living a brain-healthy lifestyle today can help reduce the risk of developing Alzheimer’s disease and related dementias tomorrow.
Research suggests that 4 in 10 cases of dementia disease may be preventable by adopting specific habits. Because Alzheimer’s can begin to develop 20-30 years before the onset of symptoms, there is no better time than NOW to start building a more dementia-resistant brain.
We’ve broken it down for you in 5 easy steps.






Ideas for Engaging with your Person through Alzheimer’s






While everyone is different, dementia-related behaviors most often stem from one of three types of triggers: emotional, physical, and environmental.
You can manage dementia-related behaviors with pharmacological (medication) or non-pharmacological approaches.
Managing Change
Be open with the medical professionals on your squad.
Track your person’s changes over time.
Give yourself permission to ask for help.
Maintain a Routine
Support a Balanced Diet
Focus on Hydration
Minimize Distractions
Adapt to Preferences
Record and Observe
Seek Professional Help


Following Traditional Approval of LEQEMBI® (lecanemab-irmb), Eisai has created new resources to provide information and support to patients and their care partners around diagnosis and treatment. These resources can be found on www.LEQEMBI.com
The Eisai Patient Support Program is also available and offers assistance programs that help people prescribed LEQEMBI and their care partners:
Understand their insurance coverage
Identify financial support programs for eligible patients
Know what to expect each step of the treatment journey
Participants may contact the Eisai Patient Support Program by visiting www.eisaipatientsupport.com/leqembi or by calling 1-833-453-7362, Monday-Friday, 8 AM to 8 PM Eastern Time.
Please click here for full Prescribing Information, including Boxed WARNING.